Tutorial
These icons indicate there is something to be interacted with. Click it when you see it.
Tutorial
These icons indicate there is something to be interacted with. Click it when you see it.
touchPANEL DISCUSSION
 A visually engaging discussion designed to emulate a ‘live’ panel experience and provide clinicians with practical expert insights to address their clinical challenges. Useful tips below will show how to navigate the activity.
Close
A visually engaging discussion designed to emulate a ‘live’ panel experience and provide clinicians with practical expert insights to address their clinical challenges. Useful tips below will show how to navigate the activity.
Close
 A visually engaging discussion designed to emulate a ‘live’ panel experience and provide clinicians with practical expert insights to address their clinical challenges. Useful tips below will show how to navigate the activity.
Close
A visually engaging discussion designed to emulate a ‘live’ panel experience and provide clinicians with practical expert insights to address their clinical challenges. Useful tips below will show how to navigate the activity.
Close
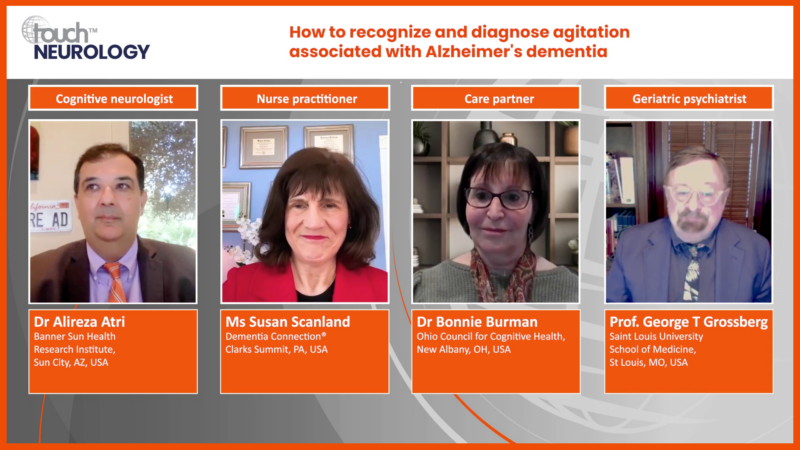
Pharmacological management of agitation in Alzheimer’s dementia: Rationale and evidence for new and emerging treatment options
Learning Objectives
After watching this activity, participants should be better able to:
- Outline best practice strategies to manage agitation in patients with Alzheimer's dementia, including psychosocial care and pharmacological treatment options
- Explain the pathophysiology of agitation in Alzheimer's dementia and the rationale for new and emerging pharmacological treatment approaches
- Evaluate evidence for new and emerging pharmacological therapies for treating agitation in Alzheimer's dementia
Overview
In this activity, three experts consider best practice in the management of agitation in Alzheimer’s dementia and the potential of new pharmacological approaches that target aspects of the underlying pathophysiology. The discussion is guided by pre-canvassed questions provided by healthcare professionals involved in the management of people living with dementia associated with Alzheimer’s disease.
This activity is jointly provided by USF Health and touchIME in collaboration with the Gerontological Society of America (GSA).
Target Audience
This activity has been designed to meet the educational needs of Alzheimer’s disease specialists, neurologists, psychiatrists, primary care physicians, specialist nurse practitioners and physician assistants involved in the management of people living with dementia associated with Alzheimer’s disease.
Disclosures
USF Health adheres to the Standards for Integrity and Independence in Accredited Continuing Education. All individuals in a position to influence content have disclosed to USF Health any financial relationship with an ineligible organization. USF Health has reviewed and mitigated all relevant financial relationships related to the content of the activity. The relevant relationships are listed below. All individuals not listed have no relevant financial relationships.
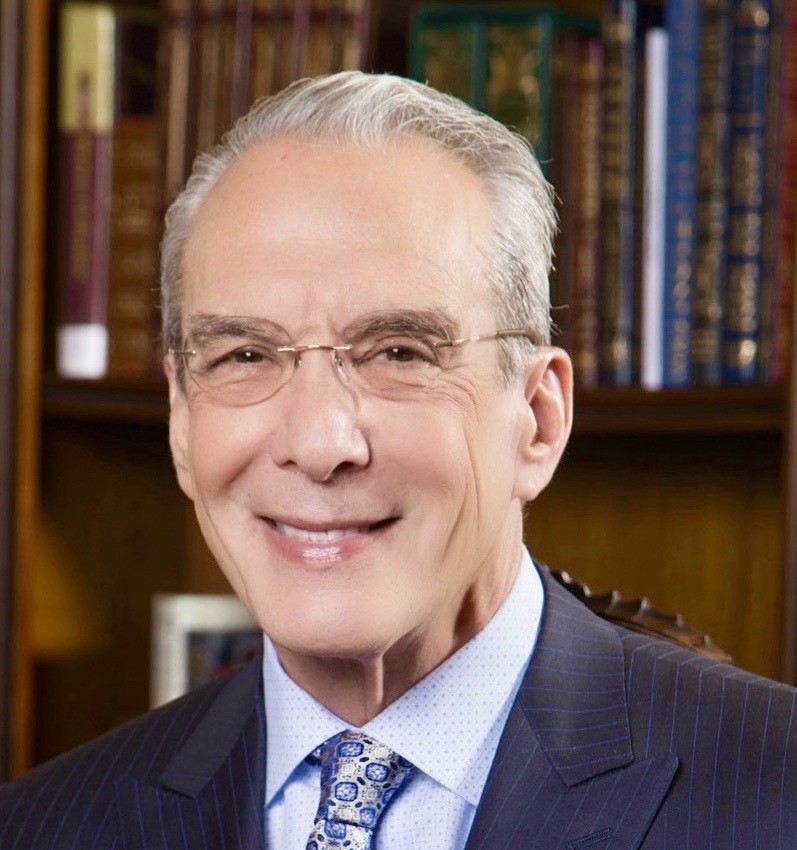
Faculty
Prof. Jeffrey Cummings discloses: Advisory board or panel fees from Acadia, Biogen, Genentech, Grifols, Janssen, Karuna, Otsuka, ReMYND, Roche and Signant Health. Consulting fees from Acadia, Acumen, ALZpath, Artery, Biogen, Biohaven, Bristol Myers Squibb, Eisai, Eli Lilly, EQT Life Sciences (formerly LSP), Fosun, GAP Foundation, Janssen, Karuna, Kinoxis, Lighthouse, Lundbeck, Merck, MoCA Cognition, New Amsterdam Pharma, Novo Nordisk, Optoceutics, Otsuka, Oxford Brain Diagnostics, Praxis, Prothena, ReMYND, Roche, Scottish Brain Sciences, Signant Health, Simcere, Sinaptica, TrueBinding and Vaxxinity. Grants/research support from the National Institute of General Medical Sciences and the National Institute on Aging. Other financial or material support from Neuropsychiatric Inventory (NPI) copyright. Stock/shareholder (self-managed) from Acumen, Alzheon, Artery, Behrens, MedAvante-Prophase and Vaxxinity.
Prof. Krista Lanctôt discloses: Advisory board or panel fees from Bright Minds, Exciva, Lundbeck, Novo Nordisk and Otsuka. Consulting fees from Bristol Myers Squibb, Cerevel Therapeutics, Exciva, Ironshore Pharma, Kondor Pharma (relationship terminated) and Praxis Therapeutics. Grants/research support from Cerevel Therapeutics. Speaker Bureau fees from Eisai Co., Ltd, Lundbeck and Novo Nordisk (all relationships terminated).
Prof. James Galvin discloses: Consulting fees from Biogen, Bristol Myers Squibb, Cognivue, Eisai, Eli Lilly, GE Healthcare, Lundbeck, Roche and Thema Medical.
Touch Medical Contributors
Christina Mackins-Crabtree has no financial interests/relationships or affiliations in relation to this activity.
USF Health Office of Continuing Professional Development and touchIME staff have no financial interests/relationships or affiliations in relation to this activity.
Requirements for Successful Completion
In order to receive credit for this activity, participants must review the content and complete the post-test and evaluation form. Statements of credit are awarded upon successful completion of the post-test and evaluation form.
If you have questions regarding credit please contact cpdsupport@usf.edu
Accreditations
Physicians
This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through a joint providership of USF Health and touchIME. USF Health is accredited by the ACCME to provide continuing medical education for physicians.
USF Health designates this enduring material for a maximum of 0.75 AMA PRA Category 1 CreditTM. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Advanced Practice Providers
Physician Assistants may claim a maximum of 0.75 Category 1 credits for completing this activity. NCCPA accepts AMA PRA Category 1 CreditTM from organizations accredited by ACCME or a recognized state medical society.
The AANPCP accepts certificates of participation for educational activities approved for AMA PRA Category 1 CreditTM by ACCME-accredited providers. APRNs who participate will receive a certificate of completion commensurate with the extent of their participation.
Date of original release: 30 October 2024. Date credits expire: 30 October 2025.
If you have any questions regarding credit, please contact cpdsupport@usf.edu
To obtain the CE/CME credit(s) from this activity, please complete this post-activity test.
Claim CreditYou may also be interested in...

REGISTER NOW FOR FREE ACCESS TO
- 1000+ topical and insightful peer-reviewed journal articles
- 100+ hours of bite-sized congress highlights
- 10 major therapy areas packed with the latest scientific advances
- 150+ specialties offering learn-on-the-go medical education
- + Concise email updates and newsletters so you never miss out

Log into your Touch Account
Earn and track your CME credits on the go, save articles for later, and follow the latest congress coverage.
Sign up with an Email
Or use a .
This Functionality is for
Members Only
Explore the latest in medical education and stay current in your field. Create a free account to track your learning.